(download as a pdf - 3.6Mb)
Compression therapy is the application of a product that applies an external force to a body area with the aim of supporting venous and lymphatic return. This support results in reduction of oedema(4), healing of venous leg ulcers(5), reduction in trophic skin changes related to chronic venous hypertension(6), and reduction in immune-complex deposition in patients with vasculitis(7).
The force can be accomplished in a number of ways including:
| What it's called | What it is | What it looks like |
| Tubular bandages | A straight, elastic, tubular bandage that is applied in three layers of separate lengths creating a pressure gradient that is greatest at the foot and ankle. |  |
| Unna Boot | General name given to a gauze bandage impregnated with zinc paste under a cohesive inelastic bandage.(5) |  |
| Short-stretch bandages | Bandages with minimal or no elastomers. Low extensibility and high stiffness.. Low resting pressure and high working pressure. (5) |  |
| Long-stretch bandages | Highly extensible (elastic) bandages that expand or contract to accommodate changes in leg geometry during walking resulting in only small pressure changes. Instead the bandage sustains applied pressures for extended periods, even when the patient is at rest.(8) |  |
| Mutliple layer bandaging | A compression system that uses one or more layer and may consist of a combination of short and long stretch bandages. |  |
| Compression garments | Specially manufactured garments that need to be individually measured and fitted. |  |
| Pneumatic compression | Pressure is applied via an inflatable garment, continuously, intermittently or in sequential cycles. (5) |  |
The images in the above table are only one example in each area. There are many other options and the ones shown above are given no particular endorsement.
“In general, bandages are most commonly used for the treatment of active VLUs; compression stockings are generally used to prevent recurrence once the ulcer has healed. “ – “Principles of compression...” pg 1 (3)
“Compression Therapy” is a therapy and the use and application of such needs to be done by health professionals who understand the underlying principles and their importance. The practitioner should seek to earn competency in the application of different forms of compression therapy. You must also work with the patient for a mutual understanding of why the therapy is required and to also explore the best form of the therapy for that patient to ensure optimum compliance. This booklet will focus on lower leg compression therapy, but the reader should be aware that compression therapy is not restricted to the lower limb.
Chronic, impaired venous return leads to leakage of proteins into the extra-cellular spaces, inflammation, and ultimately, local skin changes. These changes include ankle flair, hyperpigmentation, lipodermatosclerosis, atrophe blanché and venous eczema.
| Ankle flair | Hyperpigmentation | Venous eczema and Lipodermatosclerosis | Atrophe Blanche |
 |  |
 |
 |
Photos courtesy of DermNetNZ.org
The use of compression therapy supports venous return and reduces the impact on the skin. The compression of the tissues reduces oedema by opposing leakage of fluid from capillaries into tissues and by encouraging lymphatic drainage. It is also believed to increase the speed of venous blood flow, which may reduce local inflammatory effects.(9)
Three things impact upon the normal return of blood flow to the heart from the legs(3):
| Comparison of Arteries and Veins | ||
| Arteries | Veins | |
| Direction of blood flow | Conducts blood away from the heart | Conducts blood toward the heart |
| General appearance | Rounded | Irregular, often collapsed |
| Pressure | High | Low |
| Wall thickness | Thick | Thin |
| Valves | Not present | Present most commonly in limbs and in veins inferior to the heart |
Table modified from Anatomy & Physiology (1)

Veins are the blood vessels that return the flow of blood to the heart. The venous system is a low pressure system that utilizes valves to stop retrograde flow. Being upright during the day encourages blood to pool, especially in the lower limbs, due to the pull of gravity. This pooling increases pressure within that vein, which, in turn, puts back-pressure on the smaller veins, venules, and capillaries that feed into it. Over time the thin walls of these veins can become distorted causing their valves to no longer be able to function, increasing the incompetence of the system and further increasing the pressures. (1, 3)
The increased pressures from the incompetent venous system leads to leakage of fluids out of the capillaries and into the surrounding tissues. This is known as oedema. There are many other causes of oedema including hypertension and heart failure, severe protein deficiency, and renal failure. It is important during your assessment to determine the underlying cause to be able to create the best management plan.(1, 3)
To get the blood moving when in an upright position, blood in the lower limb is squeezed upwards by the contraction of the surrounding thigh, calf and foot muscles. This is referred to as the Calf Muscle Pump. About 90% of venous return from the legs is through this action. This is most effective during walking and ankle movement. As a result any impairment to normal calf muscle activity such as reduced ankle mobility, an abnormal gait or neurological deficit, decreases the effectiveness of this pump. Age also plays its part with calf muscle function as a result of reduced muscle bulk.(3)
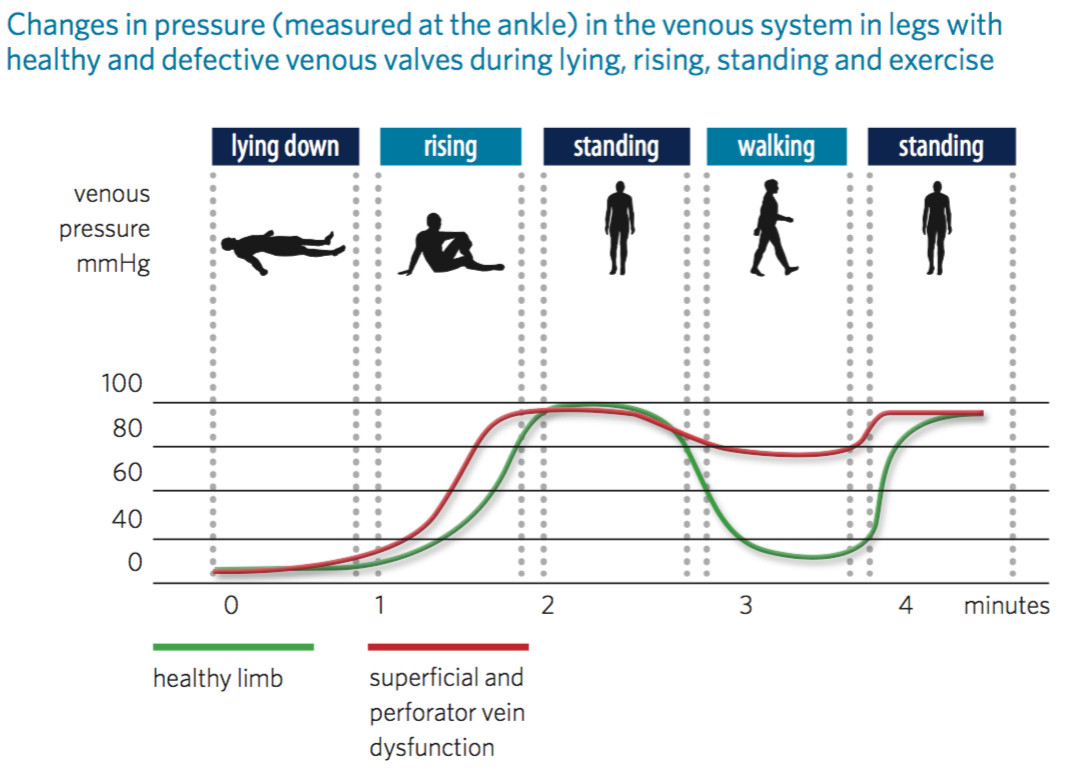
Copied from Principles of compression in venous disease(3)
There are two principles that we can apply to compression systems: Pascal’s Law and Laplace’s Law.
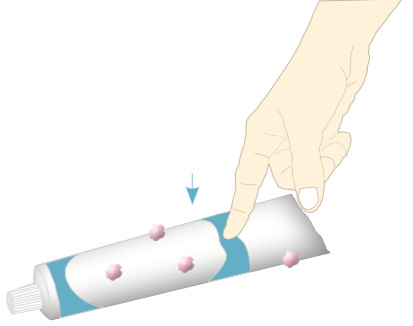
Pascal’s Law relates to rigid compression systems such as those provided by short-stretch bandaging systems and multi-layer systems that incorporate a short-stretch component. Pascal’s Law states that pressure applied to an enclosed system of an incompressible fluid is distributed evenly. See the image on the right where pressure is applied to one area of the tube of toothpaste but the toothpaste itself is extruded from all of the holes at the same rate, no matter how far away they are from the applied pressure(3). (Feel free to try this at home!)
The short-stretch bandaging acts like the rigid container. When the muscles in the leg contract they increase in circumference but are trapped within a rigid bandage. This muscle movement creates a pressure wave that is distributed evenly under the bandaging throughout the lower limb. This has a compressive effect, reducing the diameter of the veins within the lower leg and forcing the venous blood to return to the heart, producing a more normal venous pressure profile in the leg.(3)
This is particularly useful in the ambulant patient where there is a more pronounced effect (high peak pressures) during exercise. In the purely short-stretch system, with no elastic to constantly ‘squeeze’, it also means that when the muscles are not being used the resting pressures are lower, which may improve comfort. The rigid system has been shown to quickly reduce oedema, but again, without the elastic’s ability to conform, as the oedema reduces the bandage quickly becomes loose and can change its position on the leg. This can result in an unwanted distribution of pressure, possibly even dangerously increasing pressure in specific areas like the ankle. Laplace’s law can help to explain what happens to pressures when the bandaging slips and bunches up at the ankle.
Laplace’s Law relates to how we can understand what kinds of pressures are being exerted under the bandage(10). From the equation itself we can get an idea of the basic tenets. With mathematical equations, the value on the left is directly affected by the value on the right or inversely affected if the value on the right is inverted.
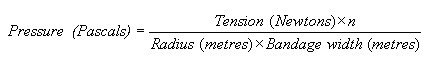
So to put it simply:
The first point relates to how much tension is in the bandage. For elastic bandaging this will vary greatly depending on how far the bandage is stretched before application. If we don’t stretch it enough the pressure will be lower, if we stretch it too much the pressure will be higher.
The second point takes into account the method we use to apply the bandage. A spiral application with 50% overlap will result in effectively applying 2 layers of the bandage, doubling the pressure. If we did a 66% overlap we would be applying 3 layers, triple the pressure! For this reason care should be taken when applying highly elastic bandages to not excessively overlap the edges.(10)
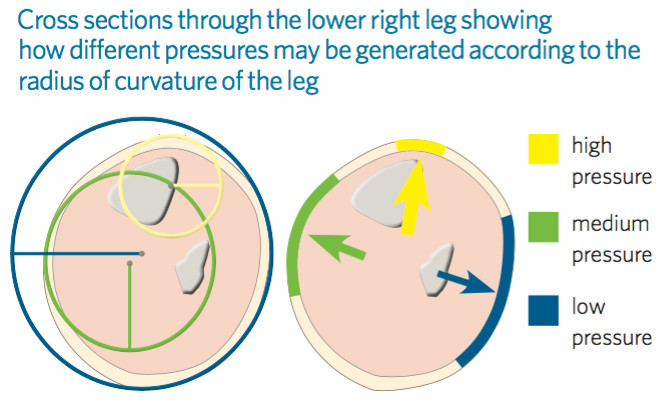
The third point says that where the radius of the leg is smaller (ie- ankle) the pressure applied by the dressing will be greater. In a perfectly shaped leg (calf:ankle = 2:1) this will result in a graduated compression from higher at the ankle to lower at the calf. But this also applies to sub-shapes within the leg. The law applies to a cylinder, but the leg is not a perfect cylinder; the tibia or malleolus may protrude. These become sub-shapes of a different (smaller) circumference than the main shape of the leg. Pressure on these areas will be higher. This is why padding of the limb is so important.
Finally, the bandage width itself will have an impact on the pressures applied. There is a mathematical formula that explains the relationship between pressure, force and area, however I think an analogy that most of us are familiar with will make more sense. Imagine you have two bags of groceries. They both have exactly the same weight of groceries in them. One is a plastic bag with those thin handles that seem to stretch and get thinner as you carry the bag home (you know the ones!). The other bag has a wider handle to carry it by. The bag with the thinner handle will tend to ‘cut in’ to your hand (or arm) so that by the time you get to where you can put them down you have red stripes where they dug in. The bag with the wider handle does not dig in. This is because the force is distributed over a wider area, effectively reducing the pressure on your hand. Where bandage kits are available in different widths, it is very important to apply it as directed.
| Type | Location | History | Ulcer Characteristics | Other findings |
Venous Leg Ulcer
|
Gaiter region of the leg; most commonly around the medial malleolus | Varicose veins DVT Other venous disease Trauma Surgery |
Irregular sloping margins Usually shallow Fibrinous, granulating base Variable size: from small to encircling the leg High exudate levels May be painful; pain relieved by elevation of the limb |
Periwound/lower limb oedema Ankle flare Varicose veins Varicose eczema Lipodermatosclerosis Hyperpigmentation Atrophie blanche |
Table copied from “Simplifying Venous Leg Ulcer Management”(9) and photo from DermNetNZ.org
VLUs are the most common type of chronic lower limb wound (40-85%) and are due to disease or disrupted function of the veins leading to a chronic venous insufficiency. There can also be some arterial insufficiency adding to the wound’s inability to heal and this is considered a mixed aetiology leg ulcer (10-20%)(9). Both of these types of ulcerations respond well to compression therapy where compression is not contra-indicated during your assessment.
| Type | Location | History | Ulcer Characteristics | Other findings |
Arterial Ulcer
|
Toes, feet or lateral or pretibial aspects of the lower leg | Intermittent claudication/rest pain Cardiac or cerebrovascular disease |
Punched out, sharply demarcated edges Painful Small and deep Necrotic wound base Dry/low exudate levels Gangrene may be present |
Surrounding skin is often dry and shiny with loss of hair Weak or absent foot pulses |
Table copied from Simplifying Venous Leg Ulcer Management(9) and photo from the Primary Care Dermatology Society
Arterial ulcers account for 5-30% of leg ulcers and are due to a disruption of the function of the arteries. The point at which microcirculation and nutrient blood flow to tissues are severely disturbed is known as critical limb ischaemia(11). These types of wounds contra-indicate the use of compression. Revascularisation, risk-factor modification and administration of antiplatelet therapy are the cornerstones of treatment for these patients. Risk reduction includes smoking cessation and treatment of hyperlipidaemia while arterial hypertension and diabetes mellitus should be adequately treated.(12)
| Type | Location | History | Ulcer Characteristics | Other findings |
Diabetic Foot Ulcer
|
Pressure bearing areas of the sole of the foot (neuropathic) Margins of the foot, e.g. over first or fifth metatarsophalangeal joints (neuroischaemic) |
Diabetes | Sensory loss when neuropathy is present Variable depth: may be deep +/- sinuses, and may involve tendons and bones |
Neuropathic: foot may be warm; ulcer often surrounded by callus Neuroischaemic: foot may be cool and foot pulses may be absent |
Table copied from “Simplifying Venous Leg Ulcer Management”(9) and photo from DermNetNZ.org
The management of diabetic foot ulcers (DFUs) focuses on the two main reasons for ulceration: neuropathy and ischaemia. As such, a multi-disciplinary team is very important, Podiatrist and/or Orthotist can look at off-loading of the DFU and the Vascular Surgeon can determine/ensure adequate blood supply. Regular debriding of wound and surrounding callous is also important as well as appropriate management for the wound itself.(13)
However, the person who has diabetes is not automagically protected from venous insufficiency. Where there is oedema or venous stasis that requires management:
“Compression may be used safely in patients with controlled diabetes. Thorough assessment of peripheral perfusion and neuropathy is essential in determining the level of risk and in selecting an appropriate compression system”- WUWHS, p10 (14)
| Type | Location(15) | History(15,16) | Ulcer Characteristics(16) | Other findings(17) |
Trophic skin changes
|
Limb/s, hands/feet, upper body (breast/chest, shoulder, back), lower body (buttocks, abdomen), genital (scrotum, penis, vulva), head, neck or face | Primary or Secondary Risk factors include cancer/cancer treatment, infection, elevated BMI, PVD, CHF, Pulmonary Hypertension, serum protein deficiency |
Grade I: the limb will swell and pit with pressure. Elevation may relieve the swelling. Grade II: the limb will become firmer, not pit, and skin changes may be noted Grade III: elephantiasis results in very thick skin and large skin folds. |
A positive Stemmer sign Presence of hyperkeratosis Enhanced skin folds developing into deep fissures especially around the ankle Papillomatosis, papules or nodules that protrude from the skin giving a cobble-stone appearance Lymphangiomas Lymphorrea |
Photos copied from from http://jamanetwork.com/journals/jamasurgery/fullarticle/394351
Oedema that develops as a result of a failure in the lymphatic system is referred to as lymphoedema. Chronic oedema is oedema that has been present for more than three months. Chronic oedema may be a result of a failure in the lymph system or it may have a more complex underlying aetiology(15). Impairment of the lymph flow can be related to pressure (capillary pressure, negative interstitial pressure, interstitial fluid colloid osmotic pressure, and plasma colloid osmotic pressure), effects on the extrinsic or intrinsic propulsion mechanisms (fibrosis impeding muscle movement) or damage to/removal of lymphatic structures (radiation or dissection of nodes)(16).
Primary lymphoedema is considered to be genetic and can be congenital lymphoedema (present from birth), lymphoedema praecox (swelling developing around puberty) or lymphoedema tarda (where it develops later in life – although it then becomes unclear if this is truly primary or a secondary lymphoedema). Secondary lymphoedemas can be caused by cancer and cancer-related treatments, and non-cancer-related conditions like chronic venous disease, trauma, heart failure, inflammation, infection, pulmonary hypertension and conditions such as arthritis. A 2005 article by Wiliams attempting to determine the extent of the condition cited an overall prevalence of 1.3 to 1.4 per 1000(15).
Compression is a major component in treatment and management of lymphoedema, along with skin care, manual lymphatic drainage and physiotherapy(4).
Given that compression therapy has such immense benefits to the majority of lower leg ulcers, why would I not use it???
The application of compression and the use of compression therapy is complex. As you can see by the science behind the bandaging, small changes in application can result large under-bandage pressure changes, potentially causing harm. Also, your assessment needs to be thorough to ensure you do not miss subtle signs that indicate the patient will not be able to tolerate the compression(18).
 |  |
| Pressure damage over the anterior tibia on a thin leg | Rupture of the distal anterior tibial tendon due to pressure damage |
Photos copied from Beldon, 2008(18)

Where arterial supply is already compromised, adding in additional pressure (be it compression therapy or anti-thromboembalism stockings) we are exacerbating the problem. But without thorough assessment we may not be aware of the problem. Also, we can not always rely on the patient to tell us if there is a problem with the bandaging, such as:
Perrin’s article in Phlebolymphology (2008)(2), while it is citing somewhat older data, is valid in it’s concerns that thorough assessment is required prior to application and that application of any compression be closely monitored.
With compression the fluid from the tissues is returned to the venous system and back into circulation. In the patient with heart failure this can lead to a risk of excessive pre-loading of the heart. It is important to introduce compression in a staged fashion, lower pressures (short-stretch) and unilaterally. Work with the Cardiologist and primary Physician to closely monitor and manage the heart failure. If the heart failure is well controlled, slowly increase compression therapy to optimum, again, in conjunction with close monitoring by their medical team(14).
In the patient with diabetes there is a risk of damage to the foot from lack of sensation or lack of blood supply to the foot that can lead to ulceration, infection and worse. Thorough neurovascular assessment is required. Where there is ischaemia – do not apply compression. Explore possible vascular investigations/interventions. Where there is neuropathy – consider using mild to moderate compression with extra padding and intermittent pneumatic compression. Always ensure diabetes is well controlled, involve the Diabetic support team and Podiatrist(14). There may be other advanced therapies (negative pressure wound therapy, biological dressings, bioengineered skin equivalents, hyperbaric oxygen therapy, platelet rich plasma and growth factors) that can also be explored where there are no other options for improving arterial supply and wounds are not improving. However these are expensive therapies and there is insufficient evidence to determine their effectiveness(19).
There are a range of documents to help you to explain compression therapy and also to guide practice with the most current and best evidence available. The guides listed below area available for download on the website. Also, always refer to your local facility’s policies regarding leg ulcer management (assessment, investigations and compression therapy).
1. OpenStax, Structure and Function of Blood Vessels, in Anatomy & Physiology2013, OpenStax.
2. Perrin, M., Skin necrosis as a complication of compression in the treatment of venous disease and in prevention of venous thromboembolism. Phlebolymphology, 2008. 15(1): p. 27-30.
3. Fletcher, J., et al., Principles of compression in venous disease: a practitioner’s guide to treatment and prevention of venous leg ulcers. Wounds International, 2013.
4. European Wound Management Association, Focus Document: Lymphoedema bandaging in practice, 2005, London: MEP Ltd.
5. Australian Wound Management Association and New Zealand Wound Care Society, Australian and New Zealand Clinical Practice Guideline for Prevention and Management of Venous Leg Ulcers.2011, Osborne Park, WA: Cambridge Publishing.
6. Whitaker, J., How to manage lower limb complications. Wounds Middle East, 2016. 3(1): p. 18-22.
7. Sinha, S.N. and P. Luk, Vasculitic leg ulcers -- a review. Primary Intention: The Australian Journal of Wound Management, 2002. 10(2): p. 79-82.
8. Marston, W. and K. Vowden, Compression Therapy: a guide to safe practice, in Position Document: Understanding Compression Therapy, European Wound Management Association, Editor 2003, Medical Education Partnership: London.
9. Harding, K., et al., Simplifying venous leg ulcer management. Consensus recommendations. Wounds International, 2015.
10. Thomas, S., The use of the Laplace equation in the calculation of sub-bandage pressure. World Wide Wounds, 2003.
11. Becker, F., et al., Chapter I: Definitions, Epidemiology, Clinical Presentation and Prognosis. European Journal of Vascular and Endovascular Surgery, 2011. 42, Supplement 2(0): p. S4-S12.
12. Diehm, N., et al., Chapter III: Management of Cardiovascular Risk Factors and Medical Therapy. European Journal of Vascular and Endovascular Surgery, 2011. 42, Supplement 2(0): p. S33-S42.
13. Edmonds, M., Diabetic foot ulcers: practical treatment recommendations. Drugs, 2006. 66(7): p. 913-929.
14. World Union of Wound Healing Societies (WUWHS), Principles of best practice: Compression in venous leg ulcers. A consensus document.2008, London: MEP Ltd.
15. Williams, A.F., P.J. Franks, and C.J. Moffatt, Lymphoedema: estimating the size of the problem. Palliative Medicine, 2005. 19(4): p. 300-313.
16. Ridner, S.H., Pathophysiology of Lymphedema. Seminars in Oncology Nursing, 2013. 29(1): p. 4-11.
17. Hampton, S., Caring for residents with chronic oedema in the lower limb. Nursing & Residential Care, 2010. 12(2): p. 70.
18. Beldon, P., Compression bandaging: avoiding pressure damage. British Journal of Community Nursing, 2008. 13(6): p. S6-S6, S8, S10-2 passim.
19. Chadwick, P., et al., International best practice guidelines: Wound management in diabetic foot ulcers. Wounds International, 2013.
20. European Wound Management Association, Position Document: Understanding Compression Therapy2003, London: MEP Ltd.
© 2015 Wound Care Resource All rights reserved | Web template modified from W3layouts