(download as a pdf - 2.1Mb)
The “real” cost is very difficult to define because costs go beyond what we see in the Hospital or health facility. There are also the personal costs, which can be quantifiable (transport, equipment, products, health care provider, lost income) and those that are more difficult to put a dollar value to (reduced quality of life, time spent managing wounds as opposed to spending it with friends or other activities). Then there’s the dual economic costs to the nation of both supporting the individual’s healing and loss of individual productivity(1).
American reports over the years have put the costs of healing a stage 4 pressure injury anywhere from around $50k to $130k USD. The wide variation may be due to what is considered included or excluded when making the calculation, but all appear to focus on hospital costs and treatment costs. One Australian study looked at the “Opportunity” cost – what could have been saved if there was no pressure injury; this looked primarily at costs related to LOS. They estimated a cost of $285M to the Australian economy in a single year(2). Recent European cost-models have indicated that the total costs of Pressure injuries may consume between 1% in the Netherlands and 4% in the United Kingdom of total health care expenditure(3).
Then there are the risks of associated complications:
Sixty thousand patients die each year from complications associated with Pressure injuries (American data)(4). Pressure injuries can delay discharge, expose the patient to potential serious infections, cause pain related to the ulcer and its treatment and is a poor indicator of mortality in an acute care setting(4).
A report by the Deloitte (a multinational company that “provide audit, consulting, financial advisory, risk management, tax, and related services to select clients”) does not dispute the cost of Pressure injuries, but it does dispute how much of it is an ‘extra’ burden to the health care system. They estimate that only 9% to 25% of all pressure injury cases result in DRG-payment increases. They explain that due to the majority of patients with pressure injuries also having numerous comorbidities, they are already reimbursed through the inclusion of the co-morbid DRGs to sufficiently to cover the extra cost of care for the pressure injury. Only when it comes to the extra costs of procedure-relevant measures such as specialised dressings, surgical interventions or vacuum therapy for the Stage 3 and 4 pressure injuries do the extra costs surface(5). Perhaps this is why in the last few years Queensland has introduced a system that penalizes hospitals for causing these injuries to patients. For a stage 3 or stage 4 pressure injury acquired in the hospital, the hospital will be fined $30k or $50k, respectively.
However, we know that the cost is more than just numbers on paper. And with the trend of ‘unsustainable’ healthcare, many countries are looking to reduce costs: pressure injuries are something which are believed to be largely preventable and very costly, and therefore an excellent place to start saving! Because of this a number of countries have started to introduce financial incentives or penalties to reduce pressure injury prevalence. The table below is a list of government programs that penalise providers for pressure injuries and/or incentivise their prevention:
| Country | Programs to Incentivise PI Prevalence | Programs that Penalise PI Occurrence |
| Belgium | - | Proposed 2015 legislation limiting payment for additional hospital days associated with hospital acquired pressure injuries |
| France | - | General accreditation and quality indicators |
| Germany | - | General accreditation and quality indicators |
| United Kingdom | Safety Thermometer (£18,525 payments each for incidence <50/1,000 inpatient discharges, assessment, care plan, reporting) | Specific quality indicators(CQIN Framework) |
| United States | Non-specific evaluation and management codes | Present on admission testingPenalty for re-admissionNever eventsFailure to reporting stages III and IV incadence penalties |
Modified from Deloitte(5)
The USA’s Centers for Medicare and Medicaid Services do not pay hospitals for the management of Pressure injuries as these are considered a medical error. Some private insurers have also followed suit. But there has also been an introduction for early detection and reporting through the use of claimable codes. Deloitte identified five “Evaluation and Management” codes that provide more than $300 for comprehensive assessment and patient evaluation, including pressure injuries. However, as of the time of writing this document I have not found evidence to indicate what change in prevalence rates has occurred since these measure have been introduced.
And while the incidence rates of stage 3 and 4 Pressure injuries appears to have reduced in QLD, it has been speculated within the Wound and Pressure Injury Prevention services at the Gold Coast that this may be due to a change in reporting and not necessarily a change in incidence. Many Pressure injuries are being reported as unstageable or suspected deep tissue injury but not re-classified at a later time. There has, however, been an increase in stage 1 and stage 2 incidence reporting. This is being seen as a positive step and has been attributed to better education and awareness campaigns; these early injuries are being noted and managed sooner.
There is potentially another cost that will start to increase here in Australia, and that’s the cost of litigation. Although this is still limited in Australia and most European countries except for the UK. In the USA and the UK litigation for pressure injury incidence common. “Litigation in the US sets benchmarks for both plaintiff-defendant win-loss ratios and settlement size: Providers lose up to 91% of pressure injury-related lawsuit and the median litigation settlement is approximately $250,000. Individual awards exceeding $300 million for pressure injury failures have occurred.”(5)
An Australian woman did succeed against both her treating doctor and a Sydney Hospital for a range of breaches of standards of care. The woman was admitted to a Sydney hospital and, over a period of time, sustained serious muscle loss following the development of a pressure injury. She was awarded $630,000 in damages in 1994.(6)
We can’t just “Do More”. Deloitte(5) has explained this very well…
“The temptation of provider managers and policy makers is to make a policy tweak here and another there: hire quality nurses, add new reporting metrics, launch awareness campaigns or provide additional training. These initiatives risk adding burden rather than addressing the systemic root causes of pressure injurys. “Do more” alienates caregivers, adds stress to lean care organizations, and typically fail to inculcate long-term changes.”
So where do we start. Awareness(5) is probably the first, and most important task we have before us. Not just our own staff but the clients, families and the general public. This is where the pressure Injury Prevention Day or the Stop The Pressure campaign in the UK help. By having more awareness it means you have more people thinking about the risks and looking for the early signs. As mentioned earlier, we have many more reports now of early stage pressure injuries and I have even had nurses complain to me about patients coming in from other facilities or the community with pressure injuries and asking “why aren’t we doing something about that!”
You may find in your organization or unit, that with all the other competing demands on your Doctor’s and Nurse’s time, that many of your own staff members remain unaware of the pressure injury prevalence rates in your hospital or your ward. Awareness is something that can be easily addressed.
The next most important thing is early detection(5). Currently, the majority of research is focused on classifying, risk assessment and management. Not enough has been targeting prevention and early detection. What we have available to us right now is our risk assessment tools and our clinical observations. But it can be difficult to identify the difference between skin irritations, sub-epidermal tissue damage and other skin-related wounds. Plus, the accuracy of the visual skin inspection relies on the educational level and skills of the staff; this means that diagnoses can be different between several staff members. As a consequence there can be inconsistent or insufficient prevention and treatment. A problem with Pressure injuries is that by the time tissue damage can be seen on the skin surface, it has already occurred at a deeper level. Patients with darker skin tones are even less likely to have a pressure injury detected early as the colour changes are less prominent. Patients with dark skin tones are more likely to be diagnosed with Stage 2-4 pressure injuries instead.
For now, we need to be diligent with our risk assessments and visual inspections to identify Pressure injuries as early as possible. As new technologies emerge there may be ways to detect sub-dermal damage before any outward signs are visible. Pressure mapping is also being used to improve prevention of Pressure injuries forming.
The nurse’s role is to do what nurses have always done, Care. 5 C’s of caring practice were proposed by Sister Simone Roach in 1987. This has since been expanded upon to 8 C’s and I’ve added one more in for good measure. Here is how they relate to pressure injury prevention and management:
| Commitment, Conscience and Compassion | These are behaviours and attitudes that define who you are as a Nurse and underpin all that you do. |
| Competence | Seek to learn, understand the underlying issues that are contributing to the pressure injury so you can develop a holistic care plan. |
| Confidence | Base your knowledge on current best practice and best evidence to know that what you are doing is right. |
| Courage | Have the courage to question what you see and do. Your questions may lead to breakthroughs in how we prevent or treat Pressure injuries. |
| Culture | Share your 9 C’s with others. Managing Pressure injuries is just one part of how we care for our patients, it’s not something special, it’s just what we do. |
| Communication | Awareness! Help others to understand what Pressure injuries are, risk factors, prevention strategies and best management plans. Ensure excellent quality documentation for your peers and help clients, family and carers to understand and help. |
| Co-operation | Factors impacting on pressure injury development and healing are multifactorial. Be pro-active and co-ordinate the care of diverse specialties as needed. |
Is there added pressure on the Nurse? This Medscape article seems to think there is while at the same time admitting that much of the situational factors impacting on the prevention of the pressure injury are outside the Nurses’ control. What does weigh heavily on the Nurse is the need for excellent documentation, as this may be called upon for both funding/penalty requirements and possibly litigation.
We have known for over 160 years how to best prevent pressure injuries:
“On guinea pigs ... I have found that no ulceration appeared when I took care to prevent any part of their bodies from being in a continued state of compression, and of washing them many times a day to remove the urine and faeces…" Henri Brown-Sequard (1853)(7)
IAD is inflammation of the skin of the perianal or genital areas, buttocks, or upper thighs due to prolonged contact with faeces, urine or sweat(10). Depending on the severity it may or may not be associated with loss of superficial skin layers and/or secondary infections(11). The presence of infection, often by opportunistic fungi, further increases morbidity(12). Differences between the two are outlined in Appendix A.
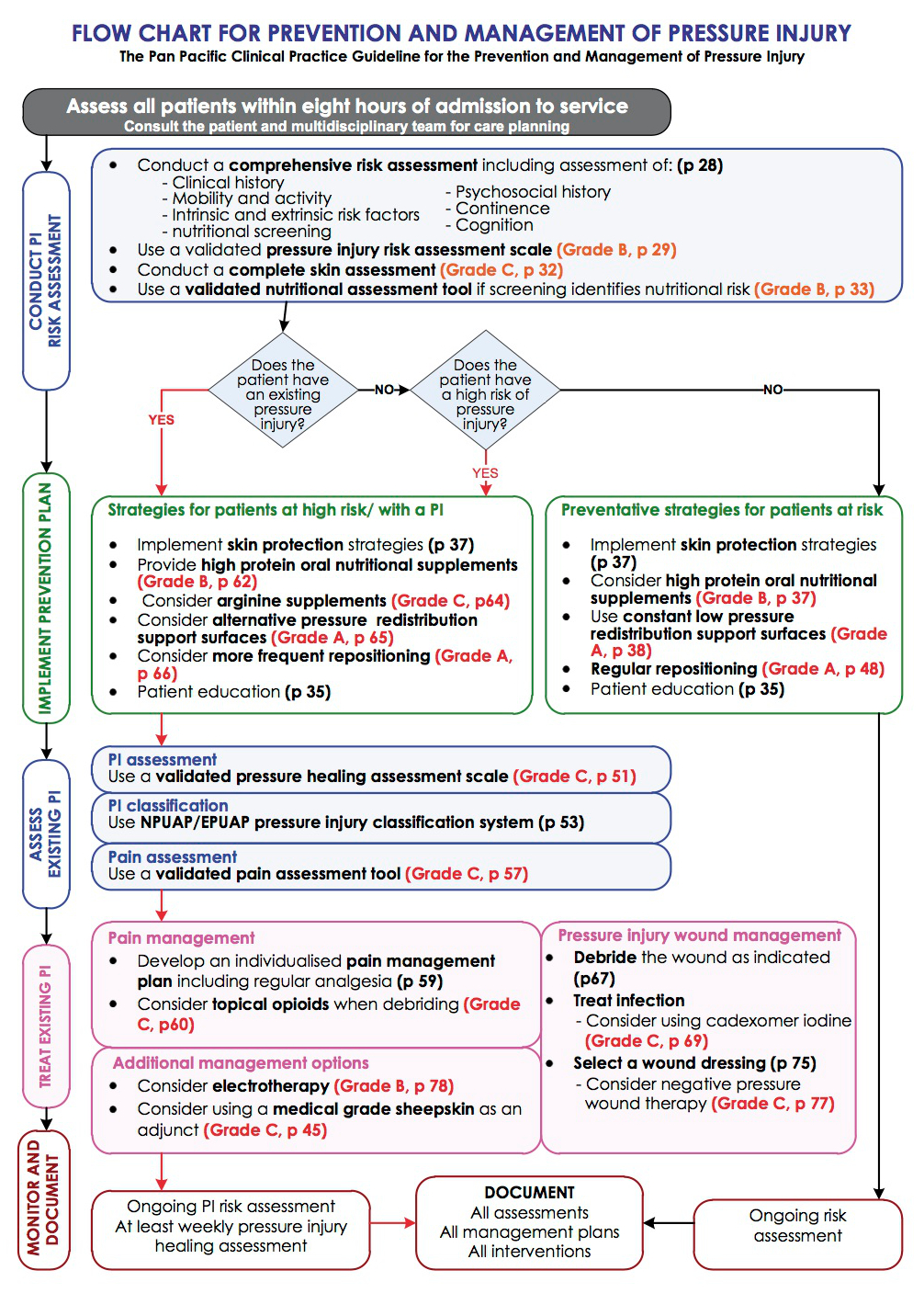
A pressure injury is a localized injury to the skin and/or underlying tissue, usually over a bony prominence, as a result of pressure or pressure in combination with shear. A number of contributing or confounding factors including, but not limited to, friction, microclimate, moisture, and nutrition are also associated with pressure injuries; the significance of these factors has yet to be elucidated(3, 8, 9). The Pan Pacific Guidelines flowchart for the prevention and management of PIs can be seen in Appendix B.
As mentioned earlier, a lot of research has gone into classification. And there is a difference in the treatment focus in that PIs are healed by removing pressure and Moisture Lesions are healed by removing moisture. However … when dealing with a sacral PI, does it really matter?
Skin that is water logged from continual wetness is more likely to breakdown, be injured by friction, be permeable to irritating substances, and be colonized by microorganisms than normal skin. Where there is a pressure injury and macerated skin, there is likely to be deterioration in the pressure injury. Where there is urine against the skin, the urine is absorbed by keratinocytes (outermost layer of skin), and when these cells are softened, they cannot provide protection from pressure injury. If the patient is also suffering from a urinary tract infection the urine will be alkaline, causing further injury to the skin’s acid mantle. Diarrhea strips the outer layer of skin, also reducing the ability of the exposed dermis to tolerate pressure. Diarrheal fluids are caustic and can damage the skin quickly. When urine is present in combination with feces, which contain bacteria and harsh gastrointestinal tract enzymes, the damage can be even quicker and more severe(13). This damage to the skin impairs the skin’s normal functioning, reducing it’s resilience. So is there some kind of relationship between IAD and PIs? Yes!
A systematic review and meta-analysis by Beekman et al (2014)(14) looked at research that included urinary incontinence, faecal incontinence, double incontinence and moisture/microenvironment and the incidence and development of pressure injuries. It showed varying strengths to the relationship between the two but generally indicated that there is a clear association that if you have IAD you are at a greater risk of developing a pressure injury. One of the articles cited in the review created interesting food for thought. It stated that in nursing homes with high rates of pressure injuries there were high rates of faecal incontinence, but in nursing homes with low rates of pressure injuries there were still high rates of faecally incontinent residents. So does this mean if we are better at managing incontinence we will we be better at managing pressure injuries, or vice versa?
Our basic principles for care remain the same, keep pressure off, keep clean, keep dry. As we learn more and more about wounds and skin in general, though, we also know that impairment is multifactorial, so always consider other contributing factors and get the support of your Multi-D teams.
Regular turning is the very foundation of pressure injury prevention. However, in the terminally ill individual, this can be frightening, painful or even harmful. Comfort and dignity are the primary objectives of the health professional providing palliative care. Appropriate use of pain control options may allow for more frequent position changes with minimal pain. However, if the patient is too sedated they will reduce how often they re-position themselves. Therefore, it is important to find just the right balance between pain management and sedation (or suppression of spontaneous movement)(13).
It is important to keep the skin intact for as long as possible. Getting the balance right for repositioning is one way. The use of specialised equipment which provides enhanced pressure redistribution and a dry and cool microclimate are also useful(13).
For those individuals who are actively dying, prevention and management of a pressure injury may be secondary to the need to promote comfort by minimizing repositioning. Involve the patient and family in the direction of their care, they may want to have help with repositioning or they may want to remain still. It is important to respect the patient's, and their family's, wishes(13).
In the final stages of life, the physiological changes happening in the body may make it impossible to prevent pressure injuries, despite the very best of preventative care. Perfusion to the tissue decrease as organs fail and even the slightest of pressures over the shortest of times will result in tissue hypoxia. In 2009, an 18-member international expert panel explored the issues and research literature surrounding end-of-life skin and wound care(15). The panel developed a consensus document entitled Skin Changes At Life’s End (SCALE). The 10 final consensus statements are(16):
Statement 1
Physiologic changes that occur as a result of the dying process (days to weeks) may affect the skin and soft tissues and may manifest as observable (objective) changes in skin color, turgor, or integrity, or as subjective symptoms such as localized pain. These changes can be unavoidable and may occur with the application of appropriate interventions that meet or exceed the standard of care.
Statement 2
The plan of care and patient response should be clearly documented and reflected in the entire medical record. Charting by exception is an appropriate method of documentation.
Statement 3
Patient centered concerns should be addressed including pain and activities of daily living.
Statement 4
Skin changes at life’s end are a reflection of compromised skin (reduced soft tissue perfusion, decreased tolerance to external insults, and impaired removal of metabolic wastes).
Statement 5
Expectations around the patient’s end of life goals and concerns should be communicated among the members of the interprofessional team and the patient’s circle of care. The discussion should include the potential for SCALE including other skin changes, skin breakdown and pressure injuries.
Statement 6
Risk factors symptoms and signs associated with SCALE have not been fully elucidated, but may include:
Statement 7
A total skin assessment should be performed regularly and document all areas of concern consistent with the wishes and condition of the patient. Pay special attention to bony prominences and skin areas with underlying cartilage. Areas of special concern include the sacrum, coccyx, ischial tuberosities, trochanters, scapulae, occiput, heels, digits, nose and ears. Describe the skin or wound abnormality exactly as assessed.
Statement 8
Consultation with a qualified health care professional is recommended for any skin changes associated with increased pain, signs of infection, skin breakdown (when the goal may be healing), and whenever the patient’s circle of care expresses a significant concern.
Statement 9
The probable skin change etiology and goals of care should be determined. Consider the 5 Ps for determining appropriate intervention strategies:
Statement 10
Patients and concerned individuals should be educated regarding SCALE and the plan of care.
| Pressure Ulcer | Moisture Lesion | Remarks | |
| Causes | Pressure and/or shear must be present. | Moisture must be present (eg, shining wet skin caused by urinary incontinence or diarrhea). | If moisture and pressure/shear are simultaneously present, the lesion could be a pressure ulcer as well as a moisture lesion (combined lesion). |
| Location | A wound not over a bony prominence is unlikely to be a pressure ulcer. | A moisture lesion may occur over a bony prominence. However, pressure and shear should be excluded as causes and moisture should be present. A combination of moisture and friction may cause moisture lesions in skin folds. A lesion that is limited to the anal cleft only and has a linear shape is not a pressure ulcer and is likely to be a moisture lesion.Perianal redness/skin irritation is most likely to be a moisture lesion resulting from faeces. | It is possible to develop a pressure ulcer where soft tissue is compressed (eg. By a nutrition tube, nasal oxygen tube or urinary catheter).Wounds in skin folds of bariatric patients may be caused by a combination of friction, moisture, and pressure.Bones may be more prominent where there is significant tissue loss (weight loss). |
| Shape | If the lesion is limited to one spot, it is likely to be a pressure ulcer.Circular wounds or wounds with a regular shape are most likely pressure ulcers; however, the possibility of friction injury has to be excluded. | Diffuse different superficial spots are more likely to be moisture lesions.In a kissing ulcer (copy lesion) at least one of the wounds is most likely caused by moisture (urine, faeces, transpiration, or wound exudate). | Irregular wound shapes are often present in a combines lesion (pressure ulcer and moisture lesion).Friction on the heels may also cause a circular lesion with full-thickness skin loss. The distinction between a friction lesion and a pressure ulcer should e made based on history and observation. |
| Depth | Partial-thickness skin loss is present when only the top layer of the skin is damaged (Stage II).In full-thickness skin loss, all skin layers are damaged (Stage III or IV).If there is a full-thickness skin loss and the muscular layer is intact, the lesion is a Stage III pressure ulcer. If the muscular layer is not intact, the lesion should be diagnosed as a Stage IV pressure ulcer. | Moisture lesions are superficial (partial-thickness skin loss).In case where the moisture lesions gets infected, the depth and extent of the lesion can be enlarged/deepened extensively. | An abrasion is caused by friction.If friction is exerted on a moisture lesion, this will result in superficial skin loss in which skin fragments are torn and jagged. |
| Necrosis | A black necrotic scab on a bony prominence is a pressure ulcer (unstageable).Necrosis can also be considered present at the heel when the skin is intact and the black/blue shimmer is visible under the skin (deep tissue injury-the lesion will most likely resolve into a necrotic eschar) | There is no necrosis in a moisture lesion. | Necrosis starts without a sharp edge but evolved into sharp edges. Necrosis softens up and changed colour (eg, blue, brown, yellow, or grey) but is never superficial.Distinction should be made between a black necrotic scab and a dried blood blister. |
| Edges | If the edges are distinct, the lesion is most likely a pressure ulcer.Wound with raised and thickened edges are old wounds. | Moisture lesions often have diffuse or irregular edges. | Jagged edges are seen in moisture lesions that have been exposed to friction. |
| Colour | Red skin:If redness is non-blanchable, this is most likely a pressure ulcer Stage I.For people with darkly pigmented skin, persistent redness may manifest as blue or purple.Red in wound bed:If there is red tissue in the wound bed, the wound is either a Stage II, a Stage III or a Stage IV pressure ulcer with granulation tissue in the wound bed.Yellow in wound bed:Softened necrosis is yellow and not superficial.Slough is a creamy, thin and superficial layer.Black in the wound bed:Black necrotic tissue in the wound bed indicates a pressure ulcer. | Red skin:If the redness is not uniformly distributed, the lesion is likely to be a moisture lesion (exclude pressure and shear as causes).Pink or white surrounding skin:Maceration resulting from moisture. | Red skin:If the skin (or lesion) is red and dry or red with a white sheen, it could be a fungal infection or intertrigo.This is often observed in the anal cleft.Green in wound bed: Infection.Be aware that zinc oxide ointments may result in whitened skin.While eosin is not recommended, it is still used in some areas. It will turn the skin red/brown and obstruct the observation of the skin. |
Modified from Pressure Ulcer Advisory Panel’s “Differentiation Between Pressure Ulcers and Moisture Lesions”(1)
1. Inernational consensus, Making the case for cost effective wound management. Wounds International, 2013.
2. Braden, B. Costs of Pressure Ulcer Prevention: Is it really cheaper than treatment? 2012 [cited 2016 January 29]; Available from: https://www.npuap.org/wp-content/uploads/2012/01/Braden-NPUAP-cost-vs-prevention-final.pdf.
3. National Pressure Ulcer Advisory Panel & European Pressure Ulcer Advisory Panel. (2009). Pressure Ulcer Treatment: Technical Report, from http://www.npuap.org
4. Hermans, M.H.E. and T. Treadwell, An Introduction to Wounds, in Microbiology of Wounds, S. Percival and K. Cutting, Editors. 2010, CRC Press: Boca Raton, Fla. p. 83-134.
5. Deloitte Consulting. Do Healthcare Systems Promote the Prevention of Pressure Ulcers? 2014 [cited 2016 January 29]; Available from: https://www2.deloitte.com/content/dam/Deloitte/be/Documents/life-sciences-health-care/2014%20White%20papers_Pressure%20ulcers_A4-7.pdf.
6. Nelson, T., Pressure ulcers in Australia: patterns of litigation and risk management issues. Primary Intention, 2003. 11(4): p. 183-187.
7. Aminoff, M.J., Brown-Sequard: An Improbable Genius Who Transformed Medicine2011, Oxford, NY: Oxford University Press.
8. Defloor, T., et al., Statement of the European Pressure Ulcer Advisory Panel -- pressure ulcer classification: differentiation between pressure ulcers and moisture lesions... including commentary by Doughty D. Journal of Wound, Ostomy & Continence Nursing, 2005. 32(5): p. 302-306.
9. The Australian Wound Management Association (AWMA) Pan Pacific Guideline Development Steering Committee, Pan Pacific Clinical Practice Guideline for the Prevention and Management of Pressure Injury.2012, Osborne Park, WA: Cambridge Media.
10. Corcoran, E. and S. Woodward, Incontinence-associated dermatitis in the elderly: treatment options. British Journal Of Nursing, 2013. 22(8): p. 450-457.
11. Denat, Y. and L. Khorshid, The effect of 2 different care products on incontinence-associated dermatitis in patients with fecal incontinence. Journal of Wound, Ostomy & Continence Nursing, 2011. 38(2): p. 171-176.
12. Bliss, D.Z., et al., Incontinence-associated dermatitis in critically ill adults: time to development, severity, and risk factors. Journal Of Wound, Ostomy, And Continence Nursing: Official Publication Of The Wound, Ostomy And Continence Nurses Society / WOCN, 2011. 38(4): p. 433-445.
13. Langemo, D.K. and J. Black, Pressure Ulcers in Individuals Receiving Palliative Care: A National Pressure Ulcer Advisory Panel White Paper. Advances in Skin & Wound Care, 2010(February): p. 59-72.
14. Beeckman, D., et al., A Systematic Review and Meta-Analysis of Incontinence-Associated Dermatitis, Incontinence, and Moisture as Risk Factors for Pressure Ulcer Development. Research in Nursing & Health, 2014. 37(3): p. 204-218.
15. Sibbald, R.G., et al., Special considerations in wound bed preparation 2011: an update. World Council of Enterostomal Therapists Journal, 2012. 32(2): p. 10-30.
16. Sibbald, R.G. and D. Krasner. SCALE: Skin changes at life's end. 2009 [cited 2016 January 29]; Available from: http://www.epuap.org/wp-content/uploads/2012/07/SCALE-Final-Version-2009.pdf.
© 2015 Wound Care Resource All rights reserved | Web template modified from W3layouts